How My Health Indicators Transformed Through Smart Rehabilitation Choices
Have you ever stared at a lab report and felt completely lost? I did—until I learned how key health indicators could guide real recovery. In rehab, numbers aren’t just data; they’re signals. From blood pressure to mobility metrics, tracking them changed everything. This is how Western medicine helped me decode my body’s feedback, make smarter choices, and see measurable progress—one indicator at a time.
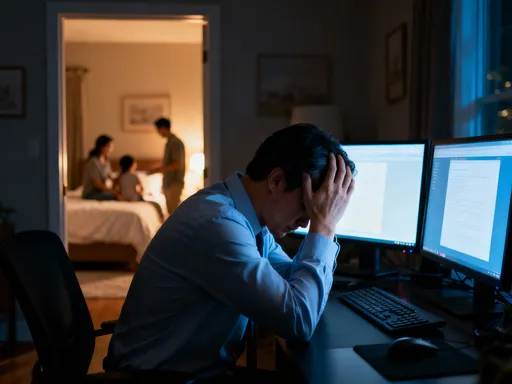
The Wake-Up Call: When Numbers Forced Me to Act
It started with a fall—nothing dramatic, just a misstep on a wet kitchen floor. But the aftermath was anything but minor. What I assumed would be a few days of soreness turned into persistent pain, limited movement, and an increasing sense of helplessness. My doctor ordered a series of tests, and when the results came back, I was handed a report filled with numbers, arrows, and abbreviations that meant nothing to me. Blood pressure was elevated, C-reactive protein (CRP) levels were high, and my resting heart rate was consistently above 90 beats per minute. These weren’t just statistics; they were red flags I could no longer ignore.
For the first time, I realized that my body was sending distress signals I had been too busy to hear. The emotional weight of those abnormal readings was overwhelming. I felt vulnerable, even afraid. But rather than spiraling into anxiety, my physical therapist helped me reframe the data—not as a list of failures, but as a starting point. Each number represented a measurable aspect of my health that could be monitored, influenced, and improved. That shift in perspective was powerful. Instead of feeling defeated, I began to see the numbers as tools. They gave me direction, a clear path forward in what had felt like a confusing and frustrating recovery process.
My rehabilitation journey officially began the day I stopped viewing these indicators as abstract medical jargon and started treating them as personal feedback. The decision to engage actively with my recovery was no longer just about following instructions—it became about understanding why those instructions mattered. With each follow-up test, I watched for changes. A slight drop in CRP meant inflammation was decreasing. A slower resting heart rate suggested improved cardiovascular efficiency. These small shifts, once invisible to me, now carried meaning. They weren’t just lab results—they were milestones.
What Are Health Indicators, Really? A No-Jargon Breakdown
Health indicators are measurable signs that provide insight into how well the body is functioning. In Western medicine, they form the foundation of clinical assessment, especially during rehabilitation. They allow healthcare providers to move beyond symptoms—how someone feels—and assess objective changes in physiology and performance. These indicators fall into several categories: vital signs, blood markers, and functional assessments. Each plays a unique role in painting a complete picture of a person’s health status.
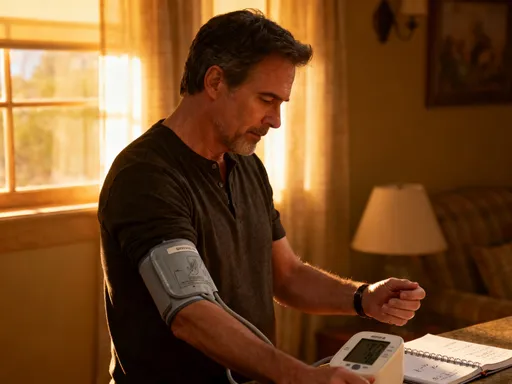
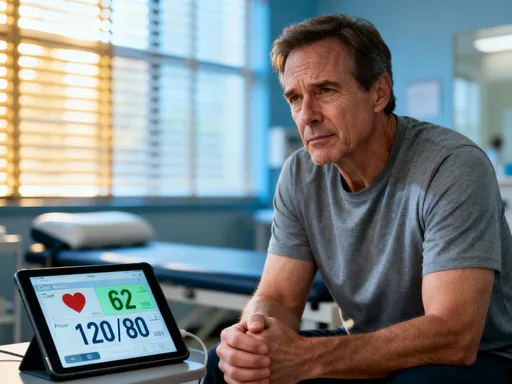
Vital signs include basic measurements like blood pressure, heart rate, respiratory rate, and body temperature. These are typically checked at every medical visit because they reflect the body’s immediate state. For example, elevated blood pressure can indicate stress, poor cardiovascular health, or inadequate recovery. In rehabilitation, tracking these over time helps determine whether the body is stabilizing or still under strain. Blood markers, on the other hand, are revealed through laboratory tests. These include cholesterol levels, blood glucose, inflammatory markers like CRP, and hormone levels. Unlike vital signs, which give a snapshot, blood markers often show trends over weeks or months, making them essential for monitoring healing and metabolic health.
Functional assessments evaluate physical ability. These might include range-of-motion tests, muscle strength evaluations, balance assessments, or gait analysis. While blood work tells clinicians what’s happening inside the body, functional tests show how well a person can move and perform daily activities. For someone recovering from an injury, this type of data is critical. It answers practical questions: Can you walk without limping? Can you lift your arm overhead? How long can you stand comfortably? Together, these three types of indicators—vital signs, blood markers, and functional tests—create a comprehensive health profile that guides treatment decisions.
In Western medicine, the reliance on such indicators is rooted in evidence-based practice. Rather than relying solely on patient reports or subjective impressions, clinicians use measurable data to diagnose, monitor, and adjust care. This approach increases accuracy and reduces guesswork. For patients, understanding these indicators fosters greater engagement. When you know what your numbers mean, you’re better equipped to participate in your own recovery. You stop being a passive recipient of care and become an informed partner in the process.
Why Tracking Matters: From Guesswork to Precision Healing
Before I began tracking my health indicators, my recovery felt unpredictable. I would have good days and bad days, but I couldn’t explain why. Was the pain worse because I overdid it? Was I improving, or just getting used to the discomfort? Without data, it was impossible to tell. The introduction of regular monitoring transformed my experience. Suddenly, progress wasn’t just a feeling—it was something I could see, measure, and trust.
One of the most significant benefits of tracking is the ability to make precise adjustments to treatment. For example, my physical therapist used gait analysis to evaluate how I walked. Specialized cameras and pressure-sensitive mats captured subtle imbalances in my stride—details I couldn’t detect on my own. Based on this data, my therapy exercises were modified to strengthen specific muscle groups and correct movement patterns. Within weeks, my walking became more symmetrical, and my lower back pain decreased. This wouldn’t have been possible without objective measurement. Guesswork would have led to generic exercises; data led to targeted, effective interventions.
Tracking also enhances communication between patients and providers. When I brought my latest blood work or wearable device data to appointments, my care team had a clearer picture of my daily patterns. They could see if my heart rate spiked at certain times, if my sleep quality fluctuated, or if my activity levels were consistent. This allowed them to identify potential issues before they became serious. For instance, a sudden increase in resting heart rate prompted my doctor to investigate possible inflammation, leading to an early adjustment in my anti-inflammatory regimen.
Moreover, regular monitoring creates accountability and motivation. Seeing a downward trend in CRP levels or an increase in muscle strength scores provided tangible proof that my efforts were paying off. It reinforced healthy behaviors—like sticking to a sleep schedule or completing daily exercises—because I could link them directly to positive changes. This kind of feedback loop is powerful. It turns abstract goals like “get stronger” or “feel better” into concrete achievements. In rehabilitation, where progress can be slow, that sense of forward movement is invaluable.
The Core Indicators That Shaped My Recovery Journey
During my rehabilitation, several key health indicators became central to my progress. These were not random numbers but carefully selected metrics that reflected different aspects of healing. By focusing on them consistently, I gained a deeper understanding of how my body responded to treatment and lifestyle changes.
One of the first indicators I monitored was C-reactive protein (CRP), a marker of systemic inflammation. After my injury, CRP levels were significantly elevated, confirming that my body was in a state of chronic inflammation. This explained the persistent pain and fatigue I experienced. My doctor recommended dietary changes—reducing processed foods and increasing omega-3 fatty acids—and prescribed a targeted physical therapy plan. Over the next eight weeks, I had CRP tested every two weeks. Watching the numbers gradually decline—from 12 mg/L to 3 mg/L—was incredibly encouraging. It validated that the interventions were working and gave me confidence to stay the course.
Resting heart rate was another crucial metric. Normally, a healthy adult’s resting heart rate falls between 60 and 100 beats per minute. Mine had climbed to 95 after the injury, likely due to pain, stress, and reduced physical activity. As I progressed through rehab, I began tracking this daily using a wearable device. I noticed that on days when I completed my exercises and managed stress with breathing techniques, my resting heart rate dropped to the mid-70s. This improvement signaled better cardiovascular efficiency and reduced sympathetic nervous system activation. It also correlated with increased energy and improved sleep, reinforcing the connection between physical and physiological recovery.
Muscle strength was assessed using a hand-held dynamometer during physical therapy sessions. This device measures the force generated by specific muscle groups. Initially, the muscles in my injured leg showed only 60% of the strength of the uninjured side. Every two weeks, we retested, and I documented the results. Seeing strength increase to 80%, then 90%, was a powerful motivator. It wasn’t just about numbers—it meant I could climb stairs without support, walk longer distances, and feel more stable on uneven surfaces. These functional gains were direct results of measurable improvements in strength.
Range of motion (ROM) was another functional indicator that played a major role. After weeks of limited movement, my hip joint had stiffened, reducing my ability to bend and rotate. My therapist used a goniometer—a simple tool that measures joint angles—to track my progress. At the start, I could only achieve 70 degrees of hip flexion; the goal was 120. Through daily stretching and mobility exercises, I reached 110 degrees within ten weeks. Each degree represented regained freedom and reduced risk of long-term stiffness. Finally, sleep efficiency—measured as the percentage of time in bed spent actually sleeping—emerged as an unexpected but vital indicator. Poor sleep was hindering my recovery, and improving it became a priority. With better sleep hygiene and consistent routines, my sleep efficiency rose from 78% to 92%, further supporting tissue repair and cognitive function.
Working With My Medical Team: How Data Built Trust
One of the most transformative aspects of my rehabilitation was the collaborative relationship I developed with my medical team. Rather than receiving instructions in isolation, I was included in every decision. The shared use of health data created transparency and trust. My physical therapist, primary care physician, and nutritionist all had access to my test results, progress charts, and functional assessments. This multidisciplinary approach ensured that my care was coordinated and consistent.
Visual tools played a big role in our communication. My therapist created simple line graphs showing my CRP levels, resting heart rate, and strength scores over time. During appointments, we reviewed these together. Seeing the trends made discussions more meaningful. Instead of vague statements like “you seem stronger,” we could point to a 15% increase in quadriceps strength or a 20-point drop in inflammation markers. This objectivity removed ambiguity and built confidence in the treatment plan.
I also learned the importance of asking questions. When a new test was ordered, I asked why it was necessary and how the results would influence my care. When a number was outside the normal range, I sought to understand what it meant in the context of my recovery. This wasn’t about challenging my providers—it was about being an informed participant. My doctors welcomed these conversations, recognizing that an engaged patient is more likely to adhere to treatment and achieve better outcomes.
This partnership mindset changed my experience of healthcare. I no longer felt like a passive patient waiting for someone else to fix me. I was an active agent in my recovery, equipped with knowledge and supported by professionals who valued my input. The data wasn’t just for them—it was for me, too. It empowered me to make daily choices that aligned with my goals, knowing they were backed by science and expert guidance.
Tools That Helped Me Stay on Track—Without Obsession
Tracking health indicators doesn’t require expensive technology, but the right tools can make the process easier and more effective. During my rehab, I used a combination of clinical assessments, wearable devices, and digital health platforms. Each served a specific purpose, and together, they provided a balanced view of my progress.
My wearable fitness tracker monitored resting heart rate, sleep patterns, and daily activity levels. It gave me real-time feedback and helped me identify trends. For example, I noticed that on days when I walked less than 5,000 steps, my next-day pain levels were higher. This insight encouraged me to stay active, even on tough days. However, I set boundaries. I didn’t check the device constantly or let a single data point dictate my mood. I reviewed the information once a day, usually in the morning, and focused on weekly trends rather than daily fluctuations.
Clinic visits remained essential. While wearables provided useful data, they couldn’t replace professional assessments. Blood tests, gait analysis, and manual strength testing offered accuracy and context that consumer devices couldn’t match. I scheduled these appointments regularly but not excessively—every four to six weeks, depending on my progress. This balance ensured I had reliable data without becoming overwhelmed by testing.
Digital health platforms allowed me to store and share my results securely. I uploaded lab reports and therapy notes to a patient portal that my entire care team could access. This streamlined communication and reduced the need for repeated explanations. It also helped me stay organized. Instead of searching through paper files, I could quickly pull up a graph showing my CRP trend over three months.
Perhaps the most important tool was self-awareness. I learned to listen to my body and recognize when to trust the data and when to rely on how I felt. There were days when my numbers looked good, but I felt fatigued—so I rested. Other times, my mood was low, but the data showed improvement—so I celebrated the progress. Avoiding data anxiety meant respecting the information without being ruled by it. The goal wasn’t perfection; it was progress.
Beyond Recovery: Making Health Indicators a Lifelong Habit
What began as a necessity during rehabilitation has become a lasting part of my life. I no longer see health indicators as emergency signals, but as routine check-ins—like tuning a car or servicing a home. Regular blood work, annual physicals, and consistent movement assessments are now part of my wellness routine. The mindset shift has been profound: from reacting to problems to proactively maintaining balance.
The lessons from rehab extend far beyond injury recovery. I’ve applied the same principles to managing everyday stress, improving sleep, and sustaining energy. For example, I now pay attention to how diet affects my inflammation markers and how exercise influences my heart rate variability. These insights help me make informed choices before issues arise. Prevention, I’ve learned, is not passive—it’s an active process of listening and responding.
I’ve also become an advocate for health literacy among friends and family. I share my experience not to prescribe solutions, but to encourage curiosity. Understanding your health data doesn’t require a medical degree. It starts with asking questions, requesting copies of test results, and seeking clear explanations. When people feel informed, they feel empowered. And empowered individuals are more likely to take consistent, positive action.
Rehabilitation taught me that healing is not a linear process, but a journey of attention, adjustment, and resilience. Health indicators are not threats to fear, but tools to guide us. They offer clarity in uncertainty, direction in confusion, and hope in moments of doubt. By embracing them with intention and balance, we can transform recovery from a reactive struggle into a proactive path toward lasting well-being.
Rehabilitation isn’t just about healing—it’s about learning. By embracing health indicators as allies, not alarms, I gained control over my recovery in ways I never expected. This journey taught me that real progress lies not in perfection, but in paying attention. With the right guidance and mindset, anyone can turn medical data into a roadmap for lasting well-being. Always consult a qualified healthcare provider—this is my story, not a substitute for professional care.